This was the final conference I organised in my role as Associate Dean for GP Education.
The conference was held on the 14th/15th November at the Hilton Warwick. 150 GP trainers attended both days. We were fortunate to have a plethora of aupicious speakers who addressed issues of differential attainment and celebrating difference. My conference introductory speech is below.
Welcome to the annual Birmingham and Solihull GP education conference. It is a real pleasure to see you this morning. We have two days of a packed programme filled with new insights and a tremendous line up of wonderful, wise speaker. I know, as with much education, that the experience is not just what is taught, it is also what it caught, through networking and peer learning. That is the meta-cognitive stuff.
I've always felt that is extremely important.
That brings me onto rolemodels.
This sari belonged to my paternal aunt - Aunty Zamruth. She was a consultant obstetrician and gynaecologist who built and lived in an Obs & Gynea nursing home in Krishnagiri, near Bangalore, South India. As I child (on vacation) I would stay in this nursing home, because it was where the family lived. I would see how hard she worked day and night. I would see how loving she was towards her own family - Three kids and me, (she was also kind and respectful to her servants/staff workers). She would not charge poor people who needed her medical care.
She always wore a Sari to work. She was one of my first rolemodels - female, professional, skilled, knowledgeable, loving and graceful. Seeing her in action was powerful. It raised my hopes and my aspirations. It made me believe 'I could'.
I am proud of this Sari, she gifted it to me, (I asked her for it, one day when she was wearing it).
Some of you know that this is my last conference as AD. Six years as AD. My last day with HEE is in 3 weeks. I have enjoy my 13 years of postgraduate Med Ed. I am excited about the new challenges ahead, leading on Medical Professionalism at Birmingham University Medical School. As a result of my leaving some trainers and trainees have conveyed some lovely farewell feedback.
Among these (are people from mainly Asian backgrounds) saying that 'I made them believe they too can succeed'. This was unexpected feedback. I realised that I was more than just an AD job description that had the required competencies. I was something more to some people. I am touched by this. You too have this 'power'. Power to inspire and power to give hope....just by being, unapologetically, you.
I was sat in a GP school board meeting last month. The Lead employer presented data on West Midlands trainee sickness absence. The group that have taken the most sick leave are female, Asian, usually Muslim trainees with childcare responsibilities....
People
Like
Me.
Maybe when they feel overwhelmed by training and curriculum requirements and feel the odds are stacked against them what really gets them through is hope brought on by knowing someone "like them" has got through and done just fine.
Don't underestimate the power of that.
I feel some trainees feel ashamed of their cultural identity, they live two lives (their professional persona is an act).....This is not helped by the 'current climate'. (I am not allowed to talk about this because I am 'in election purdah'). How ironic and amusing that a Muslim women who choses to cover, has a 'purdah' enforced ....as a HEE employee (essentially a civil servant) who is contractually required to NOT get political in the run up to an election.
There is an important term you need to know about, that is 'Intersectional'. It refers to categories of discrimination. Some people fall in the Venn diagram intersection where they have many categories - being female, being Muslim, being Asian...if I was LGBTQ I'd have a full house.
You know, you can check you intersectionality score online. Apparently mine is 55 and it tells me that 81% of people are more privileged than me. Personally, I refuse to believe that. I am incredibly privileged & blessed in many innumerable ways ....
I feel these intersectional labels along with research evidence that associates them with low achievement, paralyses individual progress and sadly sometimes becomes a self fulfilling prophecy. Is it counterproductive? Yet it is really important to capture and prove inequality if it is happening.
What do we do? How do we navigate through these sensitivities? I am hoping these next two days will give us the current evidence and postulate how we may address the issue. We have many trainees (over 50%) who fall in intersectional categories. We have performance data that shows stark differential attainment....what CAN we do? What SHOULD we do?
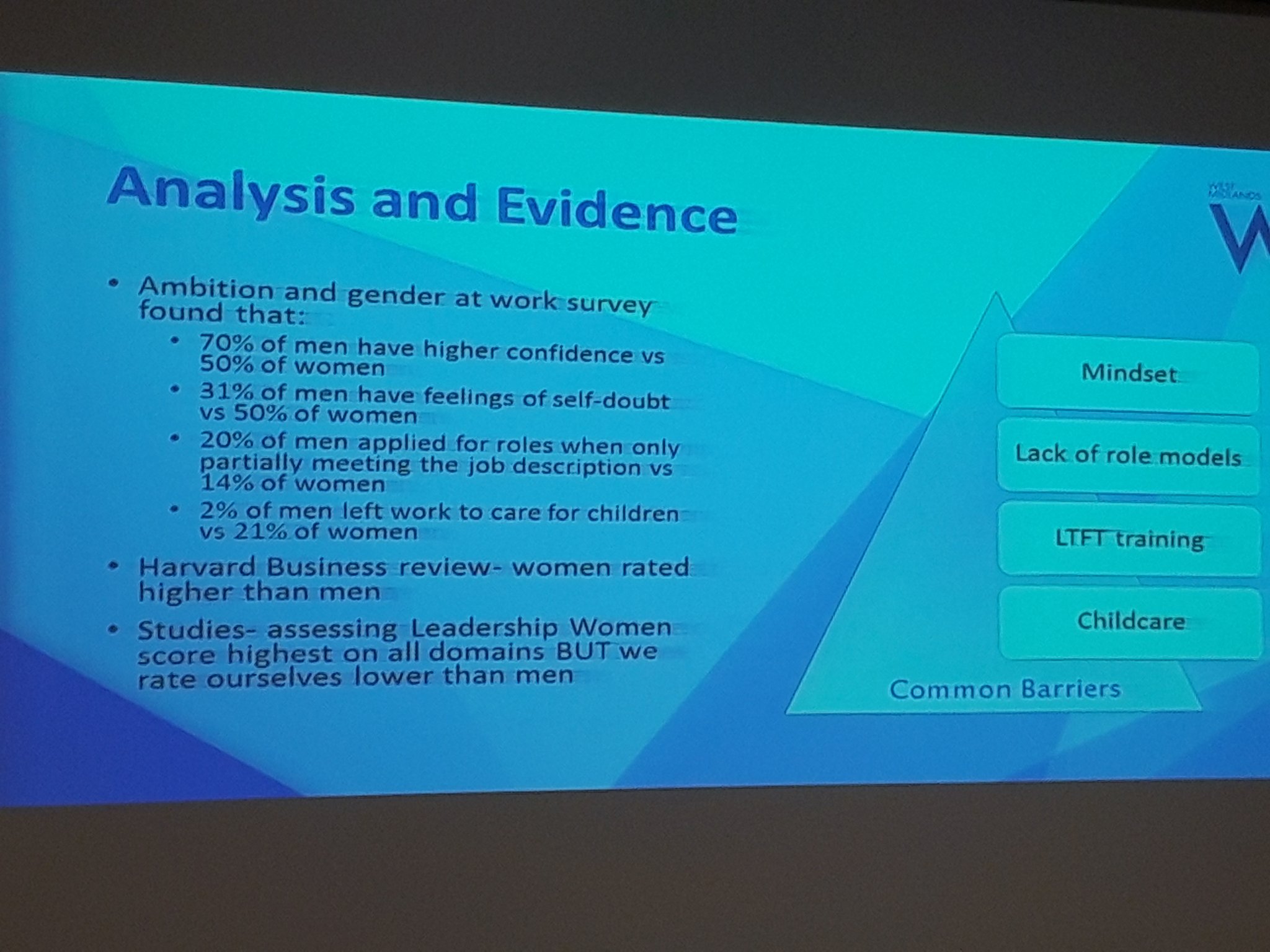
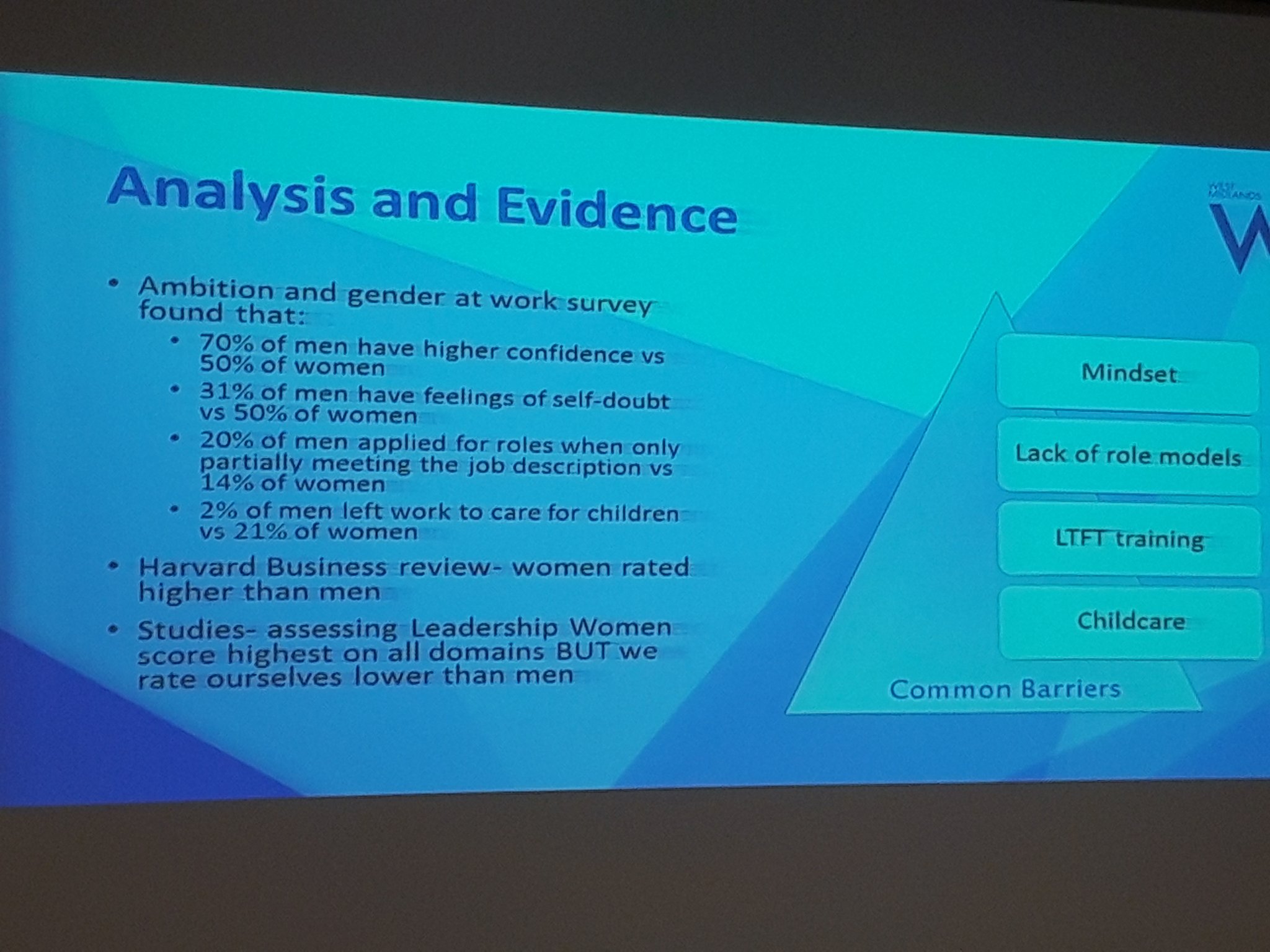
Here's some interesting data on Ambition and Gender
Dr Sarb Clare AMU Consultant, Deputy Medical Director swbnhst.
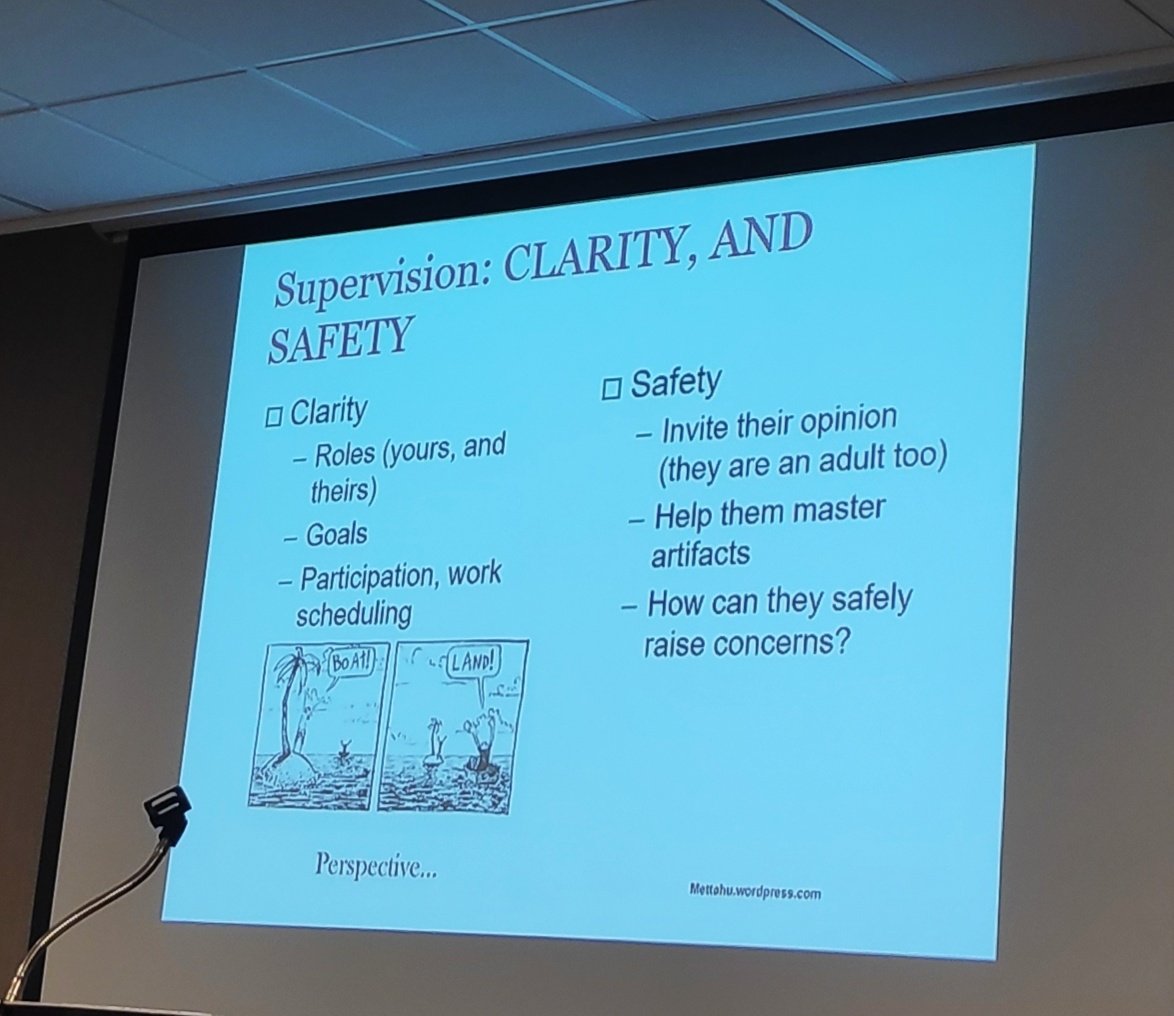
Take a minute to look and reflect on the HEE research on supervisor microaggression comments left on your tables. Have you heard these things during your career? I have.
Interesting stuff and it can undermine a person's flourishing.
I believe representation matters. There is evidence suggesting diverse boards make better decisions.
I sat on a foundation training board meeting two weeks ago. There were 17 people around the table. I was the only BAME person. In was speaking to 22 Deans from US Medical Schools on Monday. I was the only person of colour in that room.
Although I am looking forward to my new job I felt sad the representation would be even worse when leave. We also need to think and reflect whether positive discrimination/affirmative action (when it comes to recruitment) is equally 'unfair'?
The most diverse undergraduate medical training is in Manchester, Imperial and Birmingham medical schools. This is subsequently reflected in foundation training and speciality training. John Hopkins University research has shown
Studies show that students trained at diverse schools are more comfortable treating patients from a wide range of ethnic background.
It is important to develop cultural competencies in care providers to help them respect patients' values and habits, and to bridge gaps in understanding their concerns. ...
One big plus point is that as BSOL GP trainers you ARE a representative group, representative of trainees. A very gross tally (because there is no formal HEE data of this type) showed:
We have approx. 237 trainers in BSOL. 101 with English sounding surnames & 136 non English sounding surnames.
We have approx. 220 trainees currently working in BSOL. 67 with English sounding names & 153 with non-English sounding names.
When I started as a TPD in 2006 there were only two Asian TPDs (out of about 70 across the west Midlands) : Myself and Amjad Khan. (Amjad has gone onto magnificent things and is now the Director of GP Education Scotland.) Recently Steve informed me that
16 new TPDs have been appointed over last 5 years (since 2014). 12 (80%) are BAME; 11 (69%) are female; 7 (44%) are both; 100% are either. All were appointed on merit.
So, there is hope. It trickles through like sunshine on snowy white peaks. (Snowy white peaks is actually a rather tongue-in-cheek term that speaks of senior leadership in organisation including the NHS). It is basically dominated by white men. No offence Steve. You have been an incredible line manager. I have no complaints about Steve at all. He has been really empowering and encouraging to me.
I just wanted to conclude by saying that this conference is not JUST about looking at Differential Attainment and potential disadvantages from intersectional issues; it has another fundamentally important function ; That is to celebrate difference. To embrace your identity (and encourage trainees to embrace theirs), and to know that the best doctor is when the WHOLE of the doctor engages with the WHOLE of the patient.
To both feel whole and to both flourish.
It has been a pleasure and honour to serve as you AD for six year. I have met so many wonderful people and YOU inspire me everyday.
I will still be a GP trainer (if the new AD thinks I am competent enough). I look forward to being here next year, quietly sitting in the audience.
Keep going BSOL because you are awesome.
Thank you for taking a chance on me, for giving me a voice..... I feel I belong. The ovation was mind blowing! What overwhelming love I felt in that moment.


(Written on a plane flying over Greenland on 9/11/19....Literally on top of the world)